Brie Mason's Email & Phone Number
Employer Brand | Talent Attraction | Strategy | Digital | Social Media | Recruitment Marketing | Talent Community
Brie Mason Email Addresses
Brie Mason Phone Numbers
Brie Mason's Work Experience

Telstra
Employment Brand Manager
September 2011 to Present

Talent2 (onsite at Telstra Careers Centre)
Sourcing and Employment Branding Specialist
June 2010 to September 2011

Adcorp Australia
Senior Account Manager
May 2007 to June 2010

Inspired HR Limited
Marketing Manager
January 2004 to January 2006
Show more
Show less
Frequently Asked Questions about Brie Mason
What is Brie Mason email address?
Email Brie Mason at [email protected], [email protected] and [email protected]. This email is the most updated Brie Mason's email found in 2024.
How to contact Brie Mason?
To contact Brie Mason send an email to [email protected], [email protected] or [email protected].
What company does Brie Mason work for?
Brie Mason works for Telstra
What is Brie Mason's role at Telstra?
Brie Mason is Employment Brand Manager
What is Brie Mason's Phone Number?
Brie Mason's phone (**) *** *** 696
What industry does Brie Mason work in?
Brie Mason works in the Marketing & Advertising industry.
Brie Mason Email Addresses
Brie Mason Phone Numbers
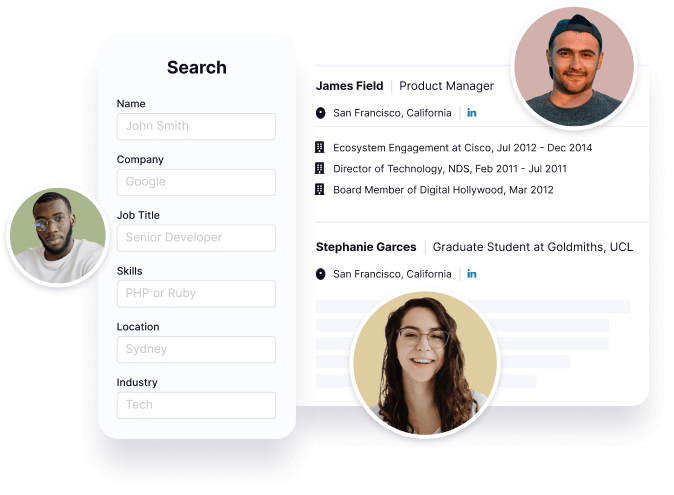
Find emails and phone numbers for 300M professionals.
Search by name, job titles, seniority, skills, location, company name, industry, company size, revenue, and other 20+ data points to reach the right people you need. Get triple-verified contact details in one-click.In a nutshell
Brie Mason's Personality Type
Extraversion (E), Intuition (N), Feeling (F), Judging (J)
Average Tenure
2 year(s), 0 month(s)
Brie Mason's Willingness to Change Jobs
Unlikely
Likely
Open to opportunity?
There's 87% chance that Brie Mason is seeking for new opportunities


































Brie Mason's Social Media Links
/in/brie-mason-9209267