Industrial Logistics Park's Email & Phone Number
Industrial & Logistics park - Burgas at Industrial & Logistics park - Burgas
Industrial Logistics Park Email Addresses
Industrial Logistics Park Phone Numbers
Industrial Logistics Park's Work Experience

Industrial & Logistics park - Burgas
Industrial & Logistics park - Burgas
January 2019 to Present

Industrial Logistic Park
Industrial
January 2012 to January 2019

Burgas
Industrial & Logistics park - Burgas - Industrial & Logistics park
Show more
Show less
Frequently Asked Questions about Industrial Logistics Park
What company does Industrial Logistics Park work for?
Industrial Logistics Park works for Burgas
What is Industrial Logistics Park's role at Burgas?
Industrial Logistics Park is Industrial & Logistics park - Burgas - Industrial & Logistics park
What is Industrial Logistics Park's personal email address?
Industrial Logistics Park's personal email address is in****[email protected]
What is Industrial Logistics Park's business email address?
Industrial Logistics Park's business email address is industrial.logisticspark@***.***
What is Industrial Logistics Park's Phone Number?
Industrial Logistics Park's phone (**) *** *** 655
What industry does Industrial Logistics Park work in?
Industrial Logistics Park works in the Construction industry.
Industrial Logistics Park Email Addresses
Industrial Logistics Park Phone Numbers
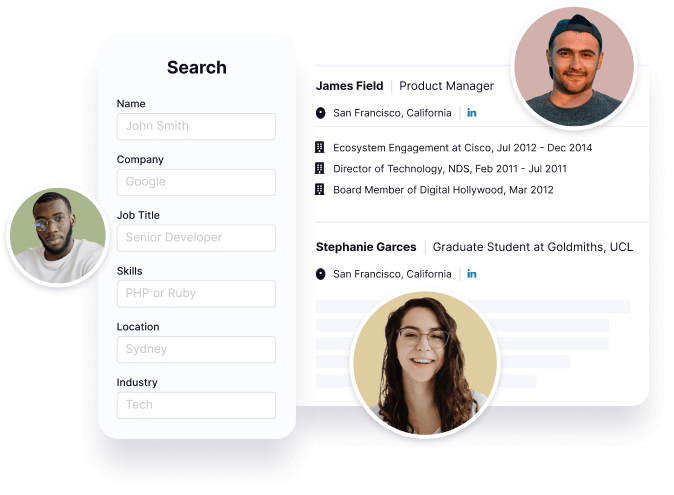
Find emails and phone numbers for 300M professionals.
Search by name, job titles, seniority, skills, location, company name, industry, company size, revenue, and other 20+ data points to reach the right people you need. Get triple-verified contact details in one-click.In a nutshell
Industrial Logistics Park's Personality Type
Extraversion (E), Intuition (N), Feeling (F), Judging (J)
Average Tenure
2 year(s), 0 month(s)
Industrial Logistics Park's Willingness to Change Jobs
Unlikely
Likely
Open to opportunity?
There's 90% chance that Industrial Logistics Park is seeking for new opportunities
Top Searched People
American screenwriter and film director
American former television journalist and talk show host
Ghanaian soccer player
American Politician
American journalist and actress


























Industrial Logistics Park's Social Media Links
/in/industrial-logistics-park-770b96198