Fahad Hassan's Email & Phone Number
Senior Business Analyst at CGI
Fahad Hassan Email Addresses
Fahad Hassan's Work Experience



Telerx
Sr. Business Systems Analyst
October 2014 to July 2015

Garda World
Business Analyst
August 2014 to October 2014

Cigna/CGI Consulting
Senior Consultant
February 2013 to August 2014

The Children's Hospital of Philadelphia
Senior Business Systems Analyst
March 2012 to February 2013


Gardner Resources Consulting, LLC
Sr. Business Systems Analyst
August 2010 to July 2011


Cognizant/ Wellpoint
Sr. Business Systems Analyst
April 2010 to August 2010

Blue Cross Blue Shields of MA
Business Systems Analyst
January 2007 to January 2010

Bahawan Cyber Tek
Business Analyst
January 2006 to January 2008

Business Systems Analyst
March 2007 to June 2007

Bahwan CyberTek, Inc.
Business Analyst Consultant
January 2005 to January 2007

AR Systems
Business Analyst
January 2006 to January 2007

Cognizant Technology Solutions
Business Analyst
January 2006 to January 2007

Ingenix
Business Analyst
January 2006 to January 2007

Business Analyst
February 2006 to May 2006

Ingenix
Business Systems Analyst
June 2005 to February 2006
Show more
Show less
Fahad Hassan's Education
Independently Studied
Certificate, IBM Certified Professional Rational Unified Process
SimpliLearn
Six Sigma White Belt Certification, Information Technology
April 2024 to April 2024
SimpliLearn
Agile Scrum Master Certification, Information Technology
April 2024 to April 2024
Centennial College
Undergrad, Computer Programming and Analysis
Show more
Show less
Frequently Asked Questions about Fahad Hassan
What company does Fahad Hassan work for?
Fahad Hassan works for CGI
What is Fahad Hassan's role at CGI?
Fahad Hassan is Employee
What is Fahad Hassan's personal email address?
Fahad Hassan's personal email address is f****[email protected]
What is Fahad Hassan's business email address?
Fahad Hassan's business email address is fahad.hassan@***.***
What is Fahad Hassan's Phone Number?
Fahad Hassan's phone (**) *** *** 410
What industry does Fahad Hassan work in?
Fahad Hassan works in the Information Technology and Services industry.
Fahad Hassan's Professional Skills Radar Chart
Based on our findings, Fahad Hassan is ...
What's on Fahad Hassan's mind?
Based on our findings, Fahad Hassan is ...
Fahad Hassan's Estimated Salary Range
Fahad Hassan Email Addresses
Find emails and phone numbers for 300M professionals.
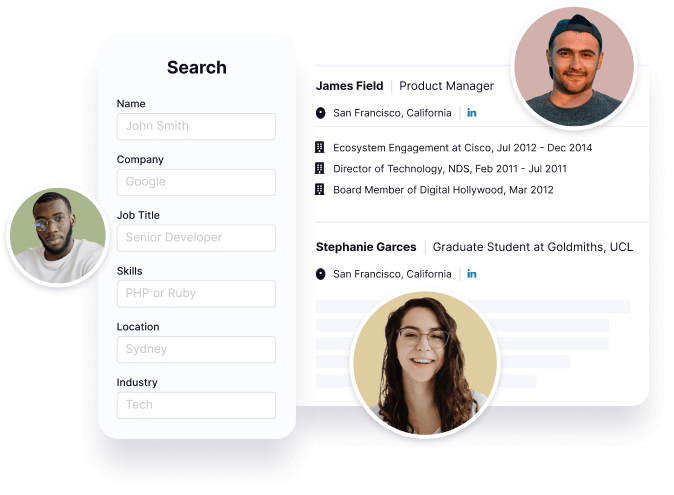
Search by name, job titles, seniority, skills, location, company name, industry, company size, revenue, and other 20+ data points to reach the right people you need. Get triple-verified contact details in one-click.In a nutshell
Fahad Hassan's Personality Type
Introversion (I), Intuition (N), Thinking (T), Judging (J)
Average Tenure
2 year(s), 0 month(s)
Fahad Hassan's Willingness to Change Jobs
Unlikely
Likely
Open to opportunity?
There's 88% chance that Fahad Hassan is seeking for new opportunities










Fahad Hassan's Social Media Links
/in/fahad-hassan-6620a61b /company/cgi